Supracondylar fracture is the commonest injury at the lower end of the humerus. This is more common in children. The management is based upon the proper knowledge of the area of the fracture, proper radiological interpretation, and care. The fracture can unite even in cases where management is not done properly but the result of this mal- handling can be the disabled limb.
Types of Fracture: The distal segment of the humerus may be displaced anteriorly or posteriorly.
Posterior displacement: This is more common and seen in 95⁰ of cases. This is also known as an extension type of fracture.
Anterior displacement: Anterior displacement of the distal segment is uncommon. This condition is known as flexion type of fracture.
MECHANISM OF INJURY
A fall on an outstretched hand transmits the force of injury to the distal end of the humerus which is displaced posteriorly following a fracture.
NATURE OF DISPLACEMENT
The fractured segment besides being posteriorly displaced is also shifted towards the lateral or medial side. The nature of displacement depends upon the nature violence and position of the limb at the time of injury.
In posterolateral displacement, the distal fracture segment is displaced posteriorly and laterally, whereas in the case of posteromedial displacement there is displacement towards the posteromedial direction. There may be an undisplaced supracondylar fracture.
SITE OF FRACTURE LINE
The fracture may pass at a variable distance from the epiphyseal line.
- Through the metaphysics: The lesion is situated at the distal end of the metaphysis. In children, this line is above the epiphysis.
- Transcondylar fracture: The fracture passes through both condyles of the humerus. Anteriorly the line runs through the coronoid fossa and posteriorly through the olecranon fossa. In children, this is immediately above the epiphyseal line.
- Epiphyseal separation: The fracture passes through the epiphyseal line. The distal segment includes the epiphyseal cartilage and the articular surface forming the elbow joint.
Diagnosis
Clinical examination: There are swelling and deformity of the elbow. The joint is in a flexed position and the forearm is supported by the patient. The triangular relation of the bony points disappear. Prominence is seen and felt posterior displacement. The circulatory efficiency is tested by nothing the color, temperature, and radial pulsation. The median nerve is the one which is injured more than the radial and ulnar nerves. Motor and sensory functions are tested.
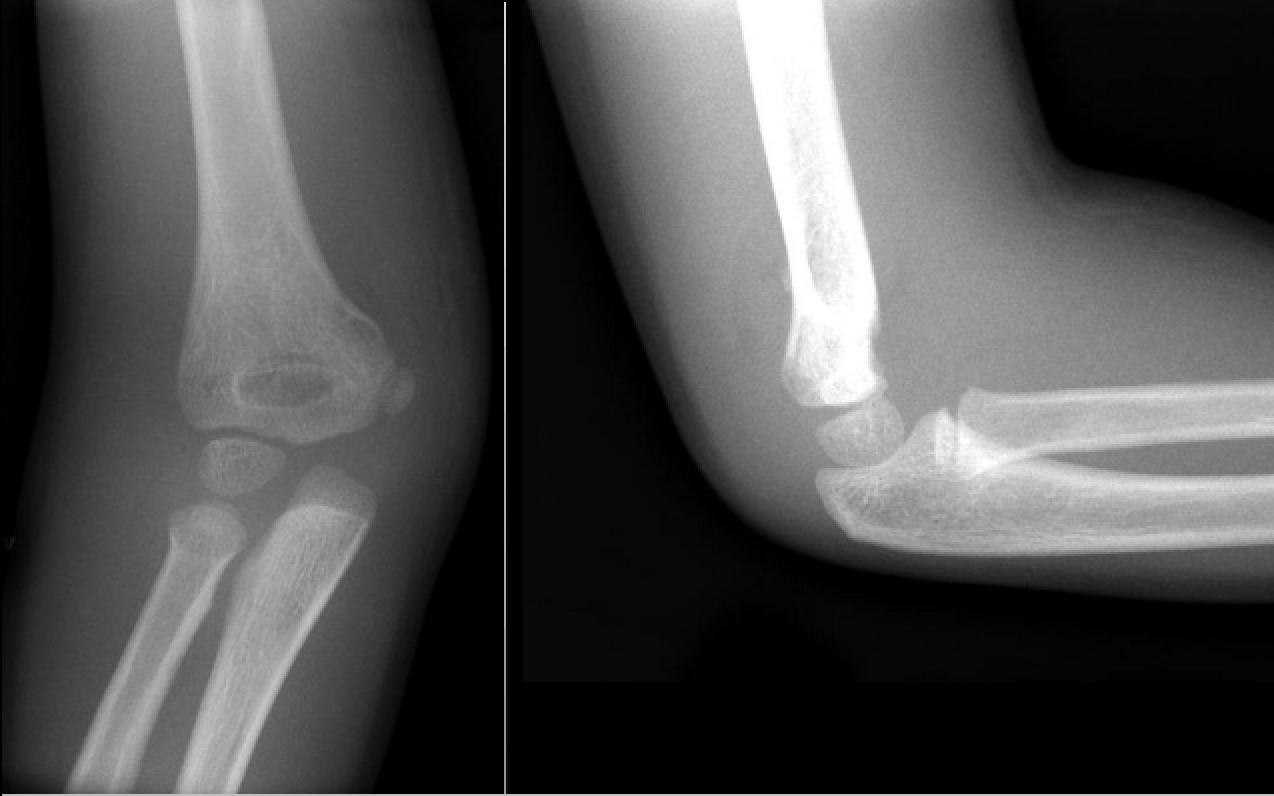
Radiological evidence: X-ray appearance confirms the nature of fracture, displacement and any associated injury to the adjoining bones and joints.
Management: Undisplaced supracondylar fracture needs no reduction. Plaster immobilization is all that is required.
SUPRACONDYLAR FRACTURE
POSTERIOR DISPLACEMENT
Pre-reduction examination: Observe the amount of swelling around the elbow and the area below. Feel for the radial pulsation and mobility of the finger joints are noted. Make a visual impression about the shortening, deformity, and type of displacement by comparing with the normal side.
Reduction: Manipulative reduction is successful in most cases. This is done under general anesthesia with the administration of muscle relaxants.
The technique of Reduction: There are three types of deformities which need to be corrected.
- Shortening.
- Posterior displacement.
- Lateral or medial displacement.
The carrying angle of the affected side is compared with the normal one. This is done before proceeding to perform the manipulation.
- Correction of shortening: Apply traction and counter traction. The surgeon exerts traction by holding the forearm while the assistant exerts traction on the arm. It is important that the forearm of the patient should be maintained in the supinated position.
- Correction of lateral displacement: Traction on the supinated forearm will correct the lateral or medial displacement to some extent. Further correction of lateral or medial displacement is made by exerting pressure on the distal end of the humerus.
- Correction of the posterior displacement: As the traction is maintained on the forearm, the elbow is flexed while pushing the distal end of the humerus forward. The elbow is flexed at an angle of more than 90⁰. The radial pulse is felt at the wrist. When pulsation is absent the elbow is made to extend from the above-flexed position till the pulsation is felt.
Plaster slab: The forearm is maintained midway between prone and supine position. The dorsal slab is applied to extend from the axilla to the metacarpal heads. The dry cotton bandage is wrapped around the plaster.
Read More:- Association Of CBD With Brain Produces Health Benefits
Check x-ray: Check x-ray is done. Remaining pulsation may be required in some cases.
Admit and observe: In doubtful cases, the patient is admitted to the hospital for observation. The circulatory condition of the limb is noted carefully. Observation for pain, pallor, paraesthesia, paralysis, and pulselessness is made. Complete the plaster when the swelling has subsided. This takes usually 2-3 days. The forearm should remain in the position midway between prone and supine.
Cases for manipulation: There is often difficulty in reducing the fracture properly. The reduction is difficult due to gross edema. In the case of a very oblique fracture when the distal segment tends to glide up even after reduction, muscles or sometimes neurovascular bundles may be interposed between the fractured segments and interfere with reduction.
Technique of manipulation
- Remanipulation must be gentle.
- When severe edema is present, manipulation may be delayed for 24-28 hours. The limb is kept elevated until the swelling subsides.
Duration of plaster: In children, plaster immobilization is usually maintained for a period of 3-4 weeks, whereas in adults, this takes a period of 6 weeks. Exercise is advised following removal of the plaster.
Immobilization by traction: Treatment by traction is indicated where gross edema is present or where circulatory impairment will develop by putting the elbow in a flexed position. Unstable fracture is another indication.
- Skeletal traction: Overhead skeletal traction is applied by inserting a pin through the subcutaneous border of the ulna, at a distance of 3 cm. from the tip of the olecranon process. Traction is maintained usually for a period of 3 weeks. Frequent x-rays are done during this period. After 3 weeks, traction is removed and the limb is immobilized in plaster with the elbow at 90⁰ for another 3 weeks.
- Skin traction: Dunlop skin traction can be applied on the forearm with the shoulder abducted at 90⁰ and the elbow- joint at 45⁰ flexion. The traction is maintained for 2½ to 3 weeks. After the release of traction, plaster immobilization is done and maintained for a period of another 3 weeks.
This article is edited by Siora Surgical team for the knowledge purpose. Siora is a top orthopedic implant manufacturing company in India. We manufacture our orthopedic implants from high-quality stainless-steel and titanium.